
CAC has been shown to lower coding time by 22% without reducing accuracy and will probably continue to be used by physician practices in an attempt to increase productivity and reduce claim backlogs. For practices, it can prompt identification of gaps in clinical documentation and faster medical billing. Patients https://www.bookstime.com/bookkeeping-services/fort-worth are now responsible for an increasing portion of their healthcare costs, requiring medical billing teams to be more focused on patient collections and insurance verification.

steps involved in the medical billing process
The emergence of multiple technologies in the healthcare industry has transitioned medical billing processes from paper-based and handwritten or typewriter-drafted documents to electronic ones. Payors can reject claims that are incorrectly coded or formatted, resulting in the claim having to be resubmitted, prolonging the process, and delaying payment. The clearinghouse formats medical claims according to each payor’s requirements, which helps payors streamline their medical billing processes. A claim can be denied if the patient didn’t get pre-authorization for a service (if applicable) or has insufficient coverage. If the claim gets denied, the patient can submit an appeal to get coverage for the costs.
What Are The Steps Involved In The Medical Billing Process And Procedures?
CareCloud’s advanced billing modules are easy to use and feature several tabs for unbilled visits, book patient appointments and more. For unbilled visits, medical teams can see which patients have been checked out but remain unbilled. When charts are signed off and go to the billing team, CareCloud’s CollectiveIQ claims scrubber cleans all claims prior to going to the clearing house.
Why Optimizing the Medical Claims Process is So Important
Understanding the medical claims process is important for both healthcare providers and patients alike. This article aims to shed light on the complex world of medical claims, explaining the terminology, the parties involved, and the challenges faced in the process. Often intertwined and confused as the same, medical billing and medical coding are different.
Review/File Claims
- In small physician practices, it’s not uncommon for the same person to serve as medical coder and medical biller.
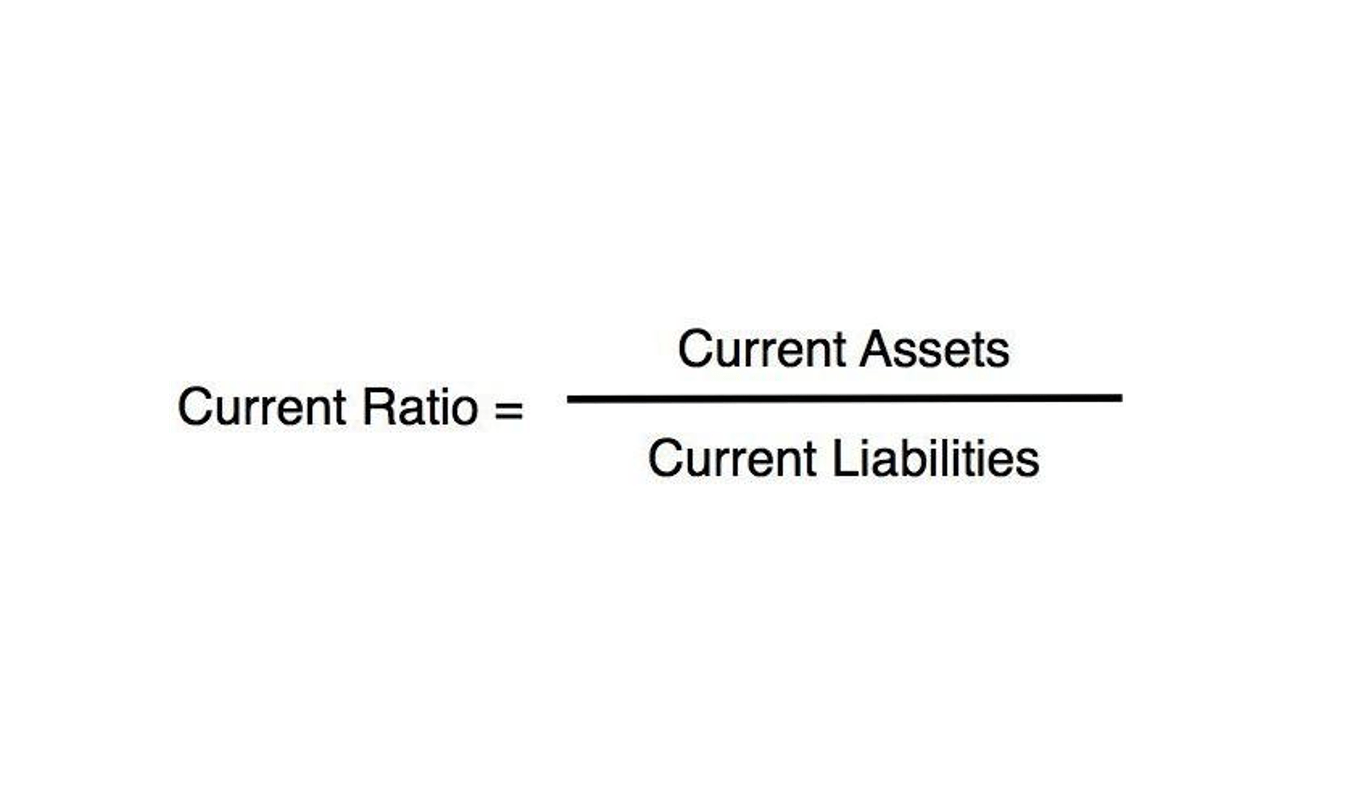
- Every stage in the medical billing process helps to reduce mistakes, streamline cash flow, and ensure insurance compliance.
- These providers can offer tailored solutions and navigate the evolving landscape of medical billing, ensuring that healthcare organizations optimize their claims process and meet the demands of the industry.
- Manual payment reconciliation is a time-consuming process that often involves tedious manual data entry and matching.
- After that, the medical biller monitors the claim to make sure their company gets paid for the services they rendered.
Additionally, bookkeeping they obtain insurance information, such as the policy number, plan details, and any secondary insurance coverage if applicable. The goal is to create a comprehensive patient profile that will serve as the foundation for the entire billing process. This process demands constant attention and diligent follow-up to ensure healthcare providers receive the compensation they deserve for their valuable work.
What is the most important part of the revenue cycle?

This document serves as the foundation for the reimbursement claim submitted to the payor. The Superbill includes essential details about the provider, the patient, and the visit, ensuring that the claim is complete and accurate for efficient processing. Medical coders are responsible for this step and they rely on two standardized coding systems to document and classify the services provided, which will eventually be put into a bill by medical billers. The second is the healthcare provider, a term that encompasses not only physicians but also hospitals, physical therapists, emergency rooms, outpatient facilities, and other entities delivering medical services. The third medical billing processing and final party is the payor, typically an insurance company, which facilitates reimbursement for the services rendered. The first step means getting the patient details down right including insurance information and medical history, both essential for accurate billing.
